What Are The 4 Stages Of Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that targets healthy joint tissues, causing pain, swelling, and reduced mobility. Unlike osteoarthritis, RA is not due to wear and tear but an immune system malfunction, leading to severe symptoms that affect daily life and quality of life.
Currently, approximately 1.3 million Americans are diagnosed with RA, with women experiencing a two to three times higher risk compared to men. Understanding the various stages of RA—including their progression, symptoms, and appropriate management strategies—is essential for those affected by this debilitating condition, enabling both patients and healthcare providers to optimize treatment plans and improve patient outcomes.
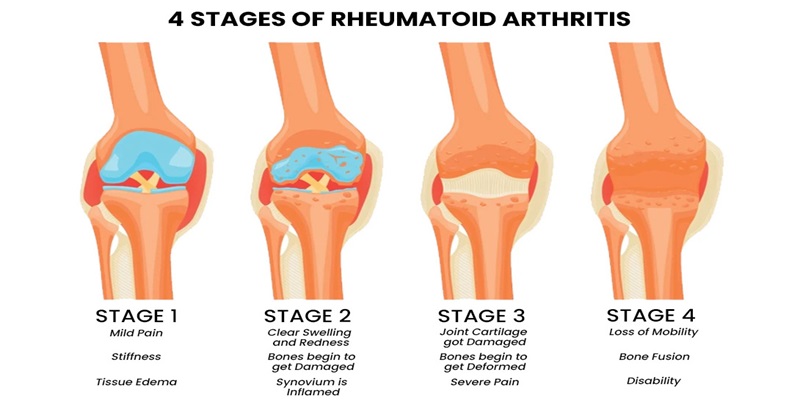
In the following sections, we will explore the four distinct stages of rheumatoid arthritis, each characterized by evolving symptoms, diagnostic criteria, and management options. From the initial stage, where symptoms may be mild and sporadic, to the more severe stages marked by significant joint damage and systemic issues, we will analyze the ramifications of each phase. By enhancing our understanding of these stages, we can significantly improve management strategies, ultimately leading to better health outcomes for those with this chronic condition.
Stage 1: Early Stage Of Rheumatoid Arthritis
Rheumatoid arthritis (RA) often begins subtly, with individuals experiencing vague yet significant symptoms. The early stage is characterized primarily by joint pain and stiffness, particularly upon waking or after prolonged periods of inactivity. Patients frequently report joint swelling, especially in the hands and feet, which can lead to discomfort and a debilitating reduction in mobility. These symptoms arise from an autoimmune process in which the immune system mistakenly attacks the synovial tissue surrounding the joints, resulting in inflammation.
This inflammatory response includes activating immune cells and releasing cytokines and enzymes, contributing to swelling and pain. This persistent inflammation can lead to progressive joint damage if not addressed promptly. Early on, the immune response orchestrates the attack on synovial tissues; however, it can also destroy cartilage without intervention.
Healthcare providers employ specific diagnostic criteria to evaluate and identify RA during this initial phase. The American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) provides guidelines that include clinical evaluations of joint involvement, serological tests for rheumatoid factor (RF) and anti-citrullinated protein antibodies (ACPAs), and assessments of inflammatory markers like C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR). Timely detection is crucial since early diagnosis allows for the initiation of treatment modalities designed to halt disease progression.
Early detection and intervention hold paramount importance in managing RA effectively. Research indicates that starting disease-modifying antirheumatic drugs (DMARDs) early in the disease can significantly reduce joint damage and enhance long-term outcomes. Additionally, monitoring and addressing other health risks associated with RA, such as cardiovascular disease, become more manageable during the early stages. By understanding and acting on these initial signs, patients can better manage symptoms and maintain a higher quality of life.
Stage 2: Moderate Stage Of Rheumatoid Arthritis
As rheumatoid arthritis (RA) progresses, the moderate stage represents a crucial turning point that can escalate symptoms significantly. Patients often experience intensified joint pain and swelling that becomes increasingly persistent, leading to challenges in daily activities such as walking and gripping objects. Stiffness is frequently noted, particularly in the mornings or after inactivity, and can last longer than an hour. This marked discomfort often results in alterations to mobility and a decreasing quality of life.
Imaging studies, like X-rays and ultrasounds, typically reveal early signs of joint damage, including decreased bone density and initial signs of erosion. These findings indicate that the synovial membrane and surrounding structures have been compromised due to the chronic inflammatory process. Identifying such structural damage early can guide treatment options and prove pivotal in altering the disease's course.
Complications and co-morbidities tend to surface during this moderate stage of RA, significantly impacting patients' health. With chronic inflammation, individuals face an increased risk of developing cardiovascular diseases. Patients may also experience anaemia or fatigue associated with the disease's systemic effects. Psychological concerns, including anxiety and depression, may arise while individuals cope with their changing health status and symptoms, making a comprehensive treatment approach essential.
Fortunately, various treatment options exist for managing symptoms and slowing disease progression during this stage of RA. Disease-modifying antirheumatic drugs (DMARDs), such as methotrexate, are commonly prescribed to reduce inflammation and protect against further joint damage. Additionally, some patients may be prescribed biologic DMARDs that specifically target immune system components responsible for inflammation. The appropriate choice of medication often hinges on individual responses to treatment, necessitating ongoing monitoring by healthcare providers.
In addition to pharmacological treatments, lifestyle modifications play a critical role in managing RA. Regular, low-impact exercise can help preserve joint mobility and strength, while physical therapy may assist individuals in coping with symptoms. Nutritional aspects are also paramount; an anti-inflammatory diet rich in omega-3 fatty acids and antioxidants can bolster health during this stage. Furthermore, practising Stress management techniques, such as mindfulness or meditation, can positively influence well-being, helping individuals deal with the mental strain of living with RA.
Therefore, while the moderate stage of rheumatoid arthritis poses significant challenges, comprehending the symptoms, potential complications, and effective treatment options can provide hope and enhance the quality of life for those affected. By proactively pursuing treatment and adopting lifestyle adjustments, patients can manage RA more effectively and improve their overall quality of life.
Stage 3: Severe Stage Of Rheumatoid Arthritis
The severe stage of rheumatoid arthritis (RA) marks a critical phase in the condition's progression, where patients often endure pronounced and debilitating symptoms. In this stage, individuals typically face intense joint pain and a significant loss of mobility, complicating even the most basic tasks like dressing, cooking, or walking short distances. Severe pain becomes a hallmark of this stage, overshadowing daily routines and inflicting considerable discomfort.
As the disease progresses, inflammation leads to severe joint damage, resulting in deformities, further inhibiting mobility and daily function. The psychological effects of severe RA are profound and cannot be overlooked; patients frequently experience feelings of frustration, isolation, and despair, which can contribute to heightened anxiety and depression. The emotional burden is compounded by fears of continued physical decline and a loss of independence, making mental health support critically crucial during this stage.
Joint damage becomes increasingly evident, particularly in the hands, wrists, and knees, leading to distinct deformities and a limited range of motion. Advanced imaging studies often reveal joint erosions and cysts indicative of ongoing tissue destruction, thereby threatening patients' abilities to maintain both personal and professional activities. This extensive damage significantly affects social participation and work performance, further isolating individuals and potentially leading to economic hardships.
More aggressive treatment plans are necessary to address the challenges posed by Stage 3 RA. Traditional DMARDs may no longer suffice for symptom control, necessitating the prescription of biologic agents targeting specific pathways in the immune response. Integrating various therapies is essential to alleviate symptoms and slow the disease's progression, focusing on enhancing patients' quality of life.
In some instances, surgical options may also be explored to repair or replace severely damaged joints. Though drastic, joint replacement surgeries can restore mobility and mitigate pain, offering significant improvements in life quality for patients who have exhausted other treatment avenues.
Pain management emerges as a pivotal element of care in this stage. A multifaceted approach that includes pharmacological interventions, physical therapy, and alternative treatments like acupuncture or mindfulness is highly recommended. The overarching goal is to efficiently manage pain while maintaining the highest possible quality of life.
Given these complexities, Stage 3 of rheumatoid arthritis presents daunting challenges for patients. However, with an empathetic and comprehensive treatment strategy that addresses both physical and psychological needs, healthcare providers can foster an environment of hope and empowerment, enabling individuals to navigate this chronic condition with as much dignity as possible.
Stage 4: Advanced Stage Of Rheumatoid Arthritis
The advanced stage of rheumatoid arthritis (RA) indicates a critical phase characterized by extensive joint damage and debilitating symptoms. At this stage in the disease, individuals frequently experience significant persistent joint pain, deformities, and major losses of physical function. Common symptoms include swollen joints that are both painful and stiff, severely limiting a person's mobility and daily life activities.
Beyond joint degradation, patients with end-stage RA may face systemic complications that further complicate their health status. The impact of rheumatoid arthritis extends beyond just the joints, affecting vital organs such as the lungs and heart. Patients may be at increased risk of developing lung issues, including interstitial lung disease, which presents as chronic cough and shortness of breath. Additionally, the likelihood of cardiovascular-related complications rises due to constant inflammation, which can result in conditions such as pericarditis and heightened risks of heart disease.
The cumulative impact of these symptoms significantly hampers physical abilities and introduces substantial psychosocial challenges. Many patients deal with feelings of helplessness and isolation; the often debilitating nature of RA complicates routine tasks and threatens independence. The decline in quality of life at this advanced stage calls for comprehensive care strategies prioritizing physical, emotional, and social needs.
At this complex juncture, a multidisciplinary care approach becomes paramount. Close collaboration between rheumatologists, physical and occupational therapists, and mental health professionals can provide a supportive network addressing the disease's physiological and emotional aspects. Rehabilitation strategies tailored to ensure patients maintain mobility and independence are crucial; therapists may offer exercises and assistive devices to help enhance patient engagement with life despite limitations.
Palliative care is vital for individuals requiring substantial support. This specialized care focuses on alleviating symptoms, improving pain management, and providing emotional support. Palliative care providers collaborate closely with patients to design individualized care plans encompassing medication management for pain relief, emotional counselling and coordinating complex care. Such a holistic strategy can significantly enhance the patient experience during this challenging phase of RA, allowing for a focus on life quality.
Support from community resources also becomes invaluable during the advanced stage. Participation in support groups fosters a safe environment for sharing experiences and learning from individuals facing similar challenges. Educational workshops can further empower patients and caregivers with coping strategies and self-care practices geared toward mental health maintenance amid the struggle for symptom management.
In summary, while the advanced stage of rheumatoid arthritis presents significant hurdles, it creates opportunities for implementing comprehensive care strategies that can dramatically improve quality of life. Patients can navigate this intricate stage with improved ease and dignity through a concerted effort combining medical assistance, therapeutic interventions, and emotional resources. Such an integrated approach addresses the immediate needs of patients while paving the way for enhanced conditions management, ultimately facilitating better living standards in the face of adversity.

Conclusion
Reflecting on the four stages of rheumatoid arthritis—an initial flare of inflammation, subsequent infiltration, tangible joint damage, and eventual decline in function—offers insight into effectively managing this chronic condition. Each phase presents unique challenges and symptoms that require careful monitoring and personalized treatment strategies. Recognizing early signs of RA and pursuing prompt intervention can lead to significantly improved long-term health outcomes.
Early identification not only diminishes the risk of severe joint damage; it empowers patients to engage in proactive treatment plans. This awareness fosters the timely implementation of disease-modifying antirheumatic drugs (DMARDs), lifestyle adjustments, and therapeutic interventions, all of which can substantially enhance an individual's quality of life. Ongoing research is vital in expanding our comprehension of RA, paving the way for emerging treatment options such as biologics and biosimilars.
As we move into the future, the dynamic landscape of ongoing research inspires optimism among patients and caregivers alike. The commitment to discovering innovative approaches ensures vigilance in combating the progression of RA. For those affected—be it directly or through caregiving efforts—embracing the journey of understanding RA, advocating for early detection, and staying informed about evolving treatment options is crucial. United in hope and determination, we can navigate the complexities of rheumatoid arthritis and strive for a brighter tomorrow.



















